A) Placenta accreta
B) Preeclampsia
C) Renal agenesis
D) Umbilical cord prolapse
E) Uterine rupture
G) None of the above
Correct Answer

verified
Correct Answer
verified
Multiple Choice
A 48-year-old woman comes to the office due to a recurrent rash. Six months ago, a rash developed on her legs that she describes as "red patches with raised areas." The rash worsened that night with intense itching that disrupted her sleep. It spontaneously resolved over the next day. Since then, she has had repeated episodes of similar symptoms on her arms, legs, and back, each lasting 8-12 hours and occurring nearly every 2-3 weeks. She reports no trauma, insect bites, travel history, sick contacts, or changes in weight. Medical history is notable for hypertension treated with lisinopril. She does not use tobacco, alcohol, or illicit drugs. Temperature is 36.1 C (97 F) , blood pressure is 138/77 mm Hg, and pulse is 78/min. Physical examination is within normal limits. The patient brings a photo of the rash, shown in the image below, from her most recent episode 2 days ago. Complete blood count, urinalysis, erythrocyte sedimentation rate, and liver function studies are within normal limits.
 The patient is concerned about her long-term prognosis. Which of the following is the most appropriate advice for this patient?
The patient is concerned about her long-term prognosis. Which of the following is the most appropriate advice for this patient?
A) It can be life threatening and requires her to carry an epinephrine injector
B) It is not life threatening, but the symptoms are difficult to control
C) Most patients have chronic recurrent symptoms requiring lifelong preventive therapy
D) Most patients have spontaneous resolution within 2-5 years
E) She can prevent recurrent attacks with dietary modifications
G) A) and E)
Correct Answer

verified
Correct Answer
verified
Multiple Choice
A 58-year-old woman comes to the office complaining of fatigue and dry mouth over the last 4 months. She has recently been waking up 2 or 3 times a night to urinate. She has no chest pain, cough, dyspnea, abdominal pain, or diarrhea. The patient has hypertension that has been treated with losartan for many years. Her medications also include 81 mg of aspirin daily. Family history is significant for type 2 diabetes mellitus and hypertension. She does not use tobacco or alcohol. Blood pressure is 143/87 mm Hg and pulse is 76/min. The patient's body mass index is 32 kg/m2. Physical examination is unremarkable. Laboratory results are as follows: 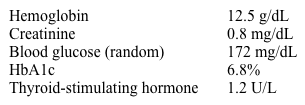 Which of the following is the best next step in management of this patient?
Which of the following is the best next step in management of this patient?
A) Diagnose patient with diabetes mellitus
B) Measure fasting blood glucose on 2 separate occasions
C) Measure random blood glucose on next visit
D) Order a glucose tolerance test
E) Order a urinalysis to detect glucosuria
G) B) and E)
Correct Answer

verified
Correct Answer
verified
Multiple Choice
A 12-year-old boy is brought to the emergency department due to unsteadiness, weakness, and falls. The patient recently went on a week-long family camping and hiking trip to the mountains in Washington State. On returning home to California 2 days ago, he experienced a sense of fatigue and a tingling sensation in his fingers. Yesterday, the patient started having bilateral leg weakness and is now unable to walk without assistance; he sways from side to side when standing and then falls to the floor. The patient has had no fever, headache, joint pain, or skin rash and has no history of recent respiratory or gastrointestinal illness. Vital signs are within normal limits. He is alert and active but can stand only briefly before requiring assistance. There is no increased resistance to neck flexion. Cranial nerve examination is normal and sensation is not impaired. Muscle strength is 4/5 in the upper extremities and 2/5 in the lower extremities. Deep tendon reflexes are absent at the knees and ankles but are normal elsewhere. Finger-to-nose testing shows dysmetria of the arms. Item 1 of 2 Which of the following is the best next diagnostic intervention that should be performed for this patient?
A) Electrodiagnostic studies
B) Imaging of the brain and spinal cord
C) Lumbar puncture and cerebrospinal fluid analysis
D) Meticulous skin examination
E) Serum analysis for bacterial toxin
G) A) and C)
Correct Answer

verified
Correct Answer
verified
Multiple Choice
A 3-day-old boy is brought to the office by his mother for a weight check. The patient was born via spontaneous vaginal delivery to a 26-year-old primigravida following an uncomplicated pregnancy. Apgar scores were 9 and 9 at 1 and 5 minutes, respectively. The patient is breastfed exclusively every 3-4 hours and sleeps approximately 15 hours a day. On physical examination, he is alert and quiet in his mother's lap. The examination is unremarkable. Anticipatory guidance is given regarding the patient's expected feeding and elimination habits, as well as upcoming developmental milestones. The topic of vaccinations is raised, and the mother adamantly states that she is unwilling to have her child vaccinated. She says, "I know you might disagree with me, but I feel that vaccines can make my son autistic. I refuse to let him be exposed to them." A prolonged discussion regarding vaccine risks and benefits does not change her beliefs. She is given additional written information regarding immunization facts. Which of the following is the best next step in management of this family?
A) Offer passive immunoprophylaxis as a substitute to vaccination
B) Plan to reopen vaccine discussion at the next visit
C) Propose an alternate vaccine schedule
D) Respect the mother's decision and discuss vaccines in the future only if requested
E) Suggest that both parents come to the next visit for further discussion
G) B) and C)
Correct Answer

verified
Correct Answer
verified
Multiple Choice
A 63-year-old woman comes to the office for a hypertension follow-up. Her blood pressure was high at her 2 previous visits despite changes in diet and exercise routine. The patient has a history of bipolar disorder with 3 hospitalizations for treatment of manic and depressive episodes. She has not been hospitalized during the past 6 years, and her symptoms have been well controlled on lithium. The patient has no other medical conditions and takes no other medications. Blood pressure is 148/90 mm Hg and pulse is 78/min. Findings from neurologic and cardiovascular examinations are within normal limits. On mental status examination, the patient is calm and speech is nonpressured. Affect is euthymic; there is no suicidal ideation. A recent serum chemistry panel, including electrolytes and renal function markers, is normal. ECG is also normal. The physician decides to prescribe an antihypertensive medication but wants to continue the patient's lithium, which is working well. Which of the following medications will be most appropriate?
A) Amlodipine
B) Hydrochlorothiazide
C) Lisinopril
D) Losartan
E) Spironolactone
G) All of the above
Correct Answer

verified
Correct Answer
verified
Multiple Choice
A 59-year-old man comes to the office for follow-up. He has a history of hypertension for which he takes 2 antihypertensive agents. The patient has no other cardiovascular problems and does not smoke. On examination, his blood pressure is 145/90 mm Hg and BMI is 25.4 kg/m2. The remainder of the examination is unremarkable. Laboratory studies show elevated fasting lipid levels, including LDL cholesterol. His 10-year risk of cardiovascular events is calculated as 10%, and a discussion regarding moderate or intensive statin therapy is initiated. The patient has read that statins may cause diabetes and asks if there is an even more increased risk with intensive compared to moderate statin therapy. Based on the abstract results with regard to incident diabetes, what is the approximate number needed to harm over 1 year for intensive compared to moderate statin therapy?
A) 2
B) 7
C) 50
D) 140
E) 500
G) A) and E)
Correct Answer

verified
Correct Answer
verified
Multiple Choice
A 32-year-old woman, gravida 3 para 2, comes to the office at 10 weeks gestation to establish prenatal care. She has mild nausea and anxiety and has not gained any weight during the pregnancy because of decreased food intake due to the nausea. The patient's first pregnancy was complicated by hyperemesis gravidarum but her second pregnancy was uneventful. She has no medical problems and her only medication is a daily prenatal vitamin. Her mother has a thyroid nodule and her father has type 2 diabetes mellitus, hyperlipidemia, and hypertension. The patient eats a vegan diet and does not use tobacco, alcohol, or illicit drugs. Blood pressure is 126/82 mm Hg and pulse is 94/min and regular. The thyroid gland is normal. There is no lid lag or proptosis. Chest auscultation is unremarkable. Laboratory results are as follows:  Which of the following is the best next step in management of this patient?
Which of the following is the best next step in management of this patient?
A) Measure free T4
B) Measure total T3
C) Reassurance
D) Start propylthiouracil
E) Thyroid ultrasound
G) A) and B)
Correct Answer

verified
Correct Answer
verified
Multiple Choice
A 74-year-old man is brought to the emergency department after being found unconscious at home. Emergency medical personnel report that he was in complete heart block when they arrived. The patient's history is significant for a myocardial infarction 12 years ago, with subsequent congestive heart failure. He has been admitted to the hospital twice over the past 3 months, once for decompensated heart failure and once for atrial fibrillation with rapid ventricular response. In reviewing the home medications brought in by his wife, the physician notes that the patient is taking aspirin; dabigatran; furosemide; apixaban; lisinopril; extended-release metoprolol; and atenolol. The wife reports that he takes these medications regularly and they were all prescribed by his doctors. He sees a primary care physician and a cardiologist, who work within the same hospital system. The patient's son, a pharmacist, expresses disappointment after learning of his father's complete heart block and prescription for 2 different beta blockers and oral anticoagulants. Which of the following actions would be most helpful in preventing the medical error that led to this patient's outcome from occurring again in the future?
A) Arrange a meeting between the cardiologist and primary care physician
B) Discuss the patient's situation with his wife
C) Hire more pharmacists to oversee discharge planning
D) Implement electronic prescribing
E) Perform a root cause analysis
G) A) and D)
Correct Answer

verified
Correct Answer
verified
Multiple Choice
A 72-year-old man is brought to the emergency department after an episode of syncope during a family gathering. The patient was sitting in his chair after dinner and passed out briefly. There are no apparent injuries and no seizure-like activity was observed. His granddaughter says that he has had frequent episodes of dizziness in the last 2 weeks. These episodes are sometimes accompanied by confusion and are not related to physical activity or changes in position. The patient's other medical problems include coronary artery disease and hypertension. He does not use alcohol or tobacco. His medications include aspirin, lisinopril, atorvastatin, and isosorbide mononitrate. Blood pressure is 105/60 mm Hg and respirations are 14/min. The patient is fully alert and oriented. Examination reveals no neck bruits. Lung fields are clear, and no cardiac murmurs are heard. Neurologic examination is within normal limits. ECG is shown in the exhibit. 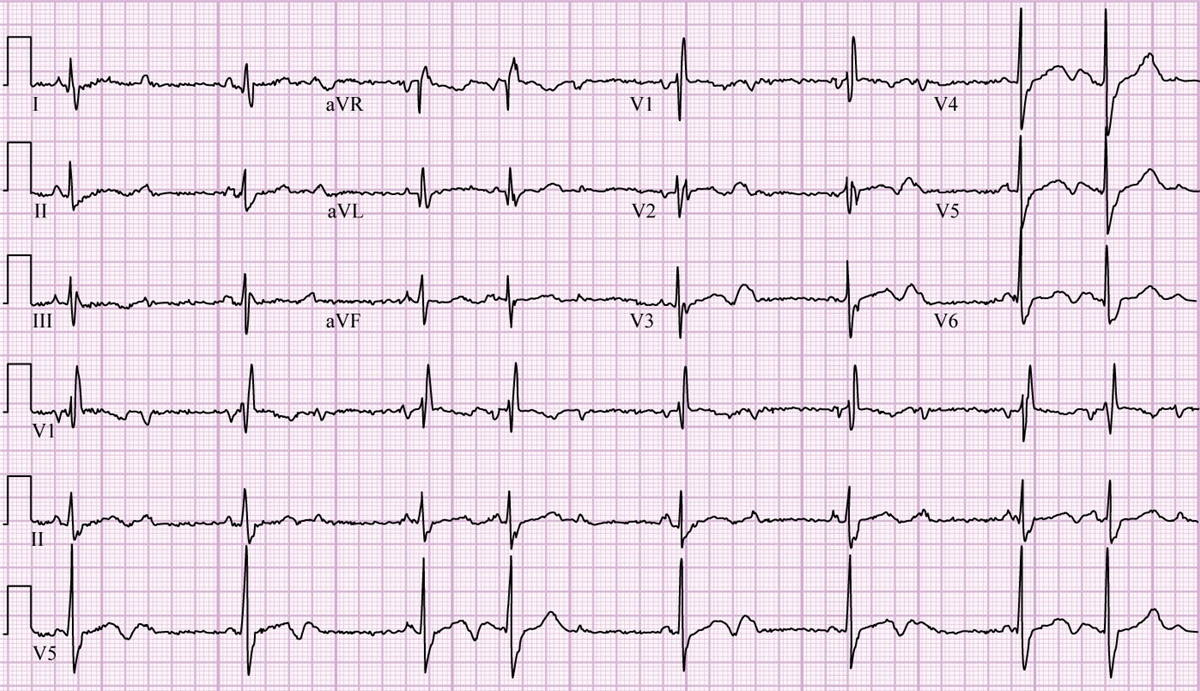 Serum potassium is 4.1 mEq/L and serum creatinine is 1.1 mg/dL. Which of the following is the best next step in management of this patient?
Serum potassium is 4.1 mEq/L and serum creatinine is 1.1 mg/dL. Which of the following is the best next step in management of this patient?
A) Arrangement for pacemaker
B) Diagnostic telemetry monitoring for 24-48 hours
C) Intravenous atropine
D) Stress testing for chronotropic competence
E) Stress testing for inducible ischemia
G) B) and E)
Correct Answer

verified
Correct Answer
verified
Multiple Choice
A 70-year-old man is brought to the emergency department by his wife after an episode of syncope while working in his garden. He regained consciousness immediately and initially refused to go to the hospital saying, "I feel fine." The patient has never experienced syncope before. According to his wife, he has always been physically active but lately has had increased fatigability; he seems to work less in the garden and spends more time indoors watching television. Medical history is significant for type 2 diabetes mellitus and gout. His only current medication is metformin. He is a lifetime nonsmoker and does not drink alcohol. Blood pressure is 100/80 mm Hg and pulse is 90/min. BMI is 28 kg/m2. Both carotid pulses are delayed. Lungs are clear on auscultation. A harsh crescendo-decrescendo murmur is heard at the base of the heart. The second heart sound is soft with an inaudible A2 component. There is no peripheral edema. ECG shows normal sinus rhythm, left ventricular hypertrophy, and secondary ST-segment and T-wave changes. Echocardiography shows concentric left ventricular hypertrophy with severe calcification of the aortic valve. The estimated aortic valve area is 0.78 cm2 and the mean transvalvular gradient is 50 mm Hg. Laboratory studies show normal complete blood count and serum creatinine of 0.8 mg/dL. Which of the following is the best statement about this patient's condition?
A) Aortic valve replacement is associated with marked reduction in mortality
B) Balloon valvulotomy is preferred due to better long-term prognosis
C) Balloon valvulotomy is preferred due to low procedural morbidity
D) Conservative treatment should be tried before offering an intervention
E) The patient's onset of symptoms has minimal bearing on his prognosis
G) C) and E)
Correct Answer

verified
Correct Answer
verified
Multiple Choice
A 23-year-old man is hospitalized for acute gastroenteritis with mild dehydration. He has type 1 diabetes mellitus that was diagnosed 6 years ago and is managed with a regimen that includes insulin glargine at bedtime and insulin aspart before meals. The patient adjusts the dose of insulin aspart based on the size of his meals and premeal glucose levels. His recent glycemic control has been excellent, with a hemoglobin A1c of 7.0%. The patient had an episode of diabetic ketoacidosis a year ago but has no chronic complications of diabetes. His glucose levels occasionally drop below 70 mg/dL, mainly at night, but he has had no symptoms or loss of consciousness due to hypoglycemia. Temperature is 36.7 C (98.1 F) , blood pressure is 114/70 mm Hg, and pulse is 100/min. Oral mucous membranes are dry, but physical examination is otherwise normal. Initial laboratory tests show a normal anion gap and a blood glucose level of 80 mg/dL. Due to frequent vomiting, the patient is able to tolerate only limited amounts of fluids or food orally, and he is started on intravenous fluids. Which of the following is the most appropriate strategy for managing this patient's insulin while he is in the hospital?
A) Continue current doses of insulin glargine and short-acting insulin
B) Decrease insulin glargine and give short-acting insulin based on glucose levels
C) Give only short-acting insulin and discontinue insulin glargine
D) Hold insulin and continue to monitor blood glucose every 6 hours
E) Initiate insulin infusion and monitor glucose every 1-2 hours
G) B) and E)
Correct Answer

verified
Correct Answer
verified
Multiple Choice
A 60-year-old man comes to the emergency department due to fever, burning on urination, generalized body aches, and lower abdominal discomfort. The dysuria began 3 days ago, and the remainder of the symptoms developed within the last 24 hours. The patient also has been unable to urinate for the past 18 hours. He has a history of hypertension, hyperlipidemia, coronary artery disease, and benign prostatic hyperplasia. Medications include aspirin, metoprolol, atorvastatin, lisinopril, and tamsulosin. He is not sexually active. The patient does not use tobacco, alcohol, or illicit drugs and has no medication allergies. Temperature is 38.3 C (100.9 F) , blood pressure is 130/75 mm Hg, pulse is 105/min, and respirations are 16/min. Abdominal examination reveals mild lower abdominal tenderness with no costovertebral angle tenderness. The urinary bladder is palpable in the hypogastric area. Rectal examination reveals a swollen, tender, and enlarged prostate with no palpable nodules. The genitals are normal in appearance and nontender to palpation. Laboratory testing shows a leukocyte count of 12,500/mm3 with 85% neutrophils and an elevated serum creatinine at 1.3 mg/dL (last known value: 0.9 mg/dL) . Microscopic urinalysis results are as follows: 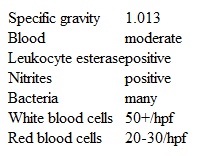 Which of the following is the best next step in management of this patient?
Which of the following is the best next step in management of this patient?
A) 5-alpha-reductase inhibitor and empiric antibiotics
B) Bladder decompression and empiric antibiotics
C) CT scan of the abdomen and pelvis
D) Prostatic massage with prostatic fluid analysis
E) Transrectal ultrasound of the prostate
G) D) and E)
Correct Answer

verified
Correct Answer
verified
Multiple Choice
A 63-year-old man comes to the office for follow-up after abnormal test results. He was found to have a blood glucose level of 255 mg/dL during a recent outpatient visit. The patient had previous normal blood glucose levels, except during a hospital admission for abdominal pain 9 months ago when he briefly required insulin for hyperglycemia. He currently feels well except for dry mouth and frequent urination, and has experienced a weight loss of 10.4 kg (23 lb) in the last 6 months. The patient has a history of obesity, hypertension, chronic pancreatitis due to alcohol abuse, obstructive sleep apnea, chronic kidney disease (estimated glomerular filtration rate 28 mL/min/1.73 m2) , and heart failure with reduced ejection fraction (ejection fraction 35%) . He quit drinking alcohol a year ago and does not use tobacco or illicit drugs. Both of his parents had type 2 diabetes mellitus; his father died of a massive myocardial infarction at age 58 and his mother died due to metastatic breast cancer. Blood pressure is 132/80 mm Hg and pulse is 76/min. BMI is 31 kg/m2. Physical examination shows mild bilateral pedal edema. Repeat blood glucose level is 250 mg/dL, and hemoglobin A1c is 9%. Which of the following medications is most appropriate for treatment of diabetes mellitus in this patient?
A) Glipizide
B) Insulin
C) Linagliptin
D) Liraglutide
E) Metformin
G) A) and B)
Correct Answer

verified
Correct Answer
verified
Multiple Choice
A 21-year-old man comes to the office due to pain and itching in his left ear. The symptoms began after a swimming party and have progressively worsened. The patient has also noted scant discharge on his pillow when waking in the morning. There is no associated hearing loss, tinnitus, or vertigo. Medical history is unremarkable and he takes no medications. Vital signs are normal without fever. Pain is elicited when the auricle is pulled superiorly or the tragus is pressed inward. The ear canal is edematous and erythematous, with soft cerumen and yellowish debris. There is no periauricular erythema or lymphadenopathy. Following gentle removal of debris from the canal under direct visualization, the tympanic membrane is fully inspected and appears normal. Which of the following is the most appropriate next step in management of this patient?
A) Prescribe antibiotic ear drops
B) Prescribe aqueous glucocorticoid drops
C) Prescribe opioid analgesic and reassure patient
D) Prescribe oral amoxicillin/clavulanate
E) Refer to otolaryngologist for wick placement
G) D) and E)
Correct Answer

verified
Correct Answer
verified
Multiple Choice
A 22-year-old man comes to the office due to difficulty concentrating and sleeping. The patient lost his job and moved in with his parents 2 months ago. Although he has been looking for work and revising his resume, he gets distracted and easily loses focus. The patient has not received any interview invitations and is worried that he will be living with his parents for a long time. He feels that he has "reverted to my high school self," playing video games most evenings and going out with friends on the weekends. The patient gets annoyed with his parents occasionally but states that he knows they are "just trying to be helpful." He has been eating more than usual since moving, gaining 3 kg (6.6 lb) and feeling tired during the day. The patient takes 2-3 hours to fall asleep each night and frequently checks the time while in bed. He drinks 3 or 4 beers a week and does not use recreational substances. Vital signs are within normal limits. Physical examination shows no abnormalities. The patient states that his mood is "okay," and he has a full range of affect. He reports no suicidal ideation. In addition to recommending psychotherapy, which of the following is the most appropriate pharmacotherapy for this patient?
A) Alprazolam
B) Lithium
C) Methylphenidate
D) Quetiapine
E) Zolpidem
G) B) and C)
Correct Answer

verified
Correct Answer
verified
Multiple Choice
A 25-year-old woman, gravida 1 para 0 aborta 1, comes to the office for a preconception counseling visit. Her sister recently developed abruptio placentae after a motor vehicle accident and underwent an emergency cesarean delivery at 32 weeks gestation. The patient had been considering stopping her oral contraceptive pills to conceive but is now feeling apprehensive about pregnancy complications after what happened to her sister. She has a history of generalized anxiety disorder and major depression. Her only surgery was a suction curettage for an elective abortion 5 years ago. In addition to oral contraceptive pills, the patient takes a selective serotonin reuptake inhibitor and multivitamin daily. Family history is noncontributory. The patient does not use alcohol, tobacco, or illicit drugs. She reports feeling safe at home. All her vaccinations are up to date. She works as a babysitter for elementary school children, with the responsibilities of driving them to after-school activities and preparing meals. The patient enjoys running and competes in 1 or 2 marathons a year. BMI is 23 kg/m2. Physical examination is within normal limits. She is considering quitting her job when she becomes pregnant and asks what else she can do to decrease her risk of complications in pregnancy. Which of the following is the best response?
A) Continue routine safety measures including wearing lap and shoulder seat belts.
B) Even though your vaccinations are up to date, you should receive the tetanus, diphtheria, and pertussis vaccination as soon as you conceive.
C) Go on bed rest during your first trimester to decrease the risk of abortion.
D) Stop working during pregnancy to limit your exposure to possible infection.
E) You will have an improved outcome if you discontinue your selective serotonin reuptake inhibitor prior to conceiving.
G) C) and D)
Correct Answer

verified
Correct Answer
verified
Multiple Choice
A 46-year-old woman comes to the office for follow-up of rheumatoid arthritis. The patient was diagnosed 2 years ago and started on treatment with prednisone and methotrexate; she had a good initial response to treatment, and the oral glucocorticoid was gradually tapered. However, her symptoms have progressively worsened over the last several months, despite increases in the methotrexate dose. The patient continues to have hand stiffness and pain lasting 2-3 hours every morning and increasing knee and ankle pain. She takes frequent doses of acetaminophen and ibuprofen but her symptoms still significantly restrict her daily activities. Medical history is otherwise unremarkable. The patient does not use tobacco, alcohol, or illicit drugs. Physical examination shows symmetric swelling and tenderness of the proximal small hand joints, wrists, and knees. Blood cell count shows mild normochromic, normocytic anemia with normal leukocyte and platelet counts. Erythrocyte sedimentation rate is 55 mm/hr. Hand x-ray reveals periarticular osteopenia and mild joint erosions. The new treatment is initiated and the patient's symptoms gradually improve. Six months later, she returns to the office with 12 hours of right knee pain. The patient has had no trauma and says, "This pain is more severe than prior arthritis flare-ups." Temperature is 38.3 C (101 F) , blood pressure is 130/80 mm Hg, pulse is 82/min, and respirations are 14/min. Right knee examination demonstrates a moderate effusion, warmth, and tenderness. Range of motion is decreased due to pain. Which of the following is the best next step in management of this patient's condition?
A) Begin oral glucocorticoid therapy
B) Obtain MRI of the knee
C) Perform arthrocentesis
D) Provide reassurance and monitor closely
E) Refer for knee replacement
G) D) and E)
Correct Answer

verified
Correct Answer
verified
Multiple Choice
An older-appearing man of unknown age is brought to the emergency department by paramedics on New Year's Eve. They found him minimally responsive and lying on the side of a street. In the emergency department, the patient's core body temperature is 29 C (84.2 F) , blood pressure is 70/30 mm Hg, heart rate is 40/min, and respirations are 6/min and shallow. His oxygen saturation is 90% on 5 L oxygen. On examination, the patient remains unresponsive to verbal stimuli and his breath smells of alcohol. His pupils are normal and symmetric but have a sluggish reaction to light. Lung examination reveals crackles bilaterally. Cardiovascular examination reveals bradycardia with an irregular pulse. Neurologic examination is difficult to perform but shows marked hyporeflexia throughout. An initial ECG shows sinus bradycardia with frequent premature ventricular complexes. Capillary blood glucose is 315 mg/dL. Paramedics have started an infusion of warmed normal saline via 16-g peripheral access. The patient has also received one dose of intravenous thiamine. Item 1 of 2 Which of the following is the most appropriate next step in management of this patient?
A) Atropine
B) Endotracheal intubation
C) Insertion of central line through subclavian vein
D) Insulin infusion
E) Intravenous furosemide
G) A) and D)
Correct Answer

verified
Correct Answer
verified
Multiple Choice
A 26-year-old man comes to the office after learning that one of his sexual partners tested positive for HIV. The patient has had intermittent headaches, malaise, nausea, and blurry vision over the last several weeks. He has had no fever, sore throat, skin rash, genital lesions, or weight loss. The patient has no prior history of sexually transmitted infections or chronic medical problems. He smokes a pack of cigarettes daily, consumes alcohol occasionally, and does not use illicit drugs. The patient has had multiple sexual partners over the last several years and does not use condoms consistently. Temperature is 37.1 C (98.8 F) , blood pressure is 122/74 mm Hg, and pulse is 72/min. There is no scleral icterus, oropharyngeal lesions, or skin rash. Mild, generalized lymphadenopathy is present. Cardiopulmonary and abdominal examinations are normal. Cranial nerves, deep tendon reflexes, and sensation are normal. No nuchal rigidity is present. Ophthalmologic examination reveals no abnormalities. Screening HIV immunoassay is positive. Other laboratory studies are as follows: 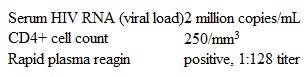 A subsequent fluorescent treponemal antibody absorption test is positive. Contrast-enhanced CT scan of the head reveals no space-occupying lesions. Several hours after the appropriate treatment for the syphilis is administered, the patient develops a fever and headache and feels "achy all over." On repeat evaluation, temperature is 38.1 C (100.6 F) , blood pressure is 130/82 mm Hg, and pulse is 105/min. The remainder of the physical examination is unchanged. Which of the following could have prevented this patient's current condition?
A subsequent fluorescent treponemal antibody absorption test is positive. Contrast-enhanced CT scan of the head reveals no space-occupying lesions. Several hours after the appropriate treatment for the syphilis is administered, the patient develops a fever and headache and feels "achy all over." On repeat evaluation, temperature is 38.1 C (100.6 F) , blood pressure is 130/82 mm Hg, and pulse is 105/min. The remainder of the physical examination is unchanged. Which of the following could have prevented this patient's current condition?
A) Assessment of drug interactions
B) Careful history-taking of allergies
C) No effective prevention is available
D) Pretreatment with antihistamines
E) Pretreatment with corticosteroids
G) D) and E)
Correct Answer

verified
Correct Answer
verified
Showing 381 - 400 of 1121
Related Exams